
Volpara has entered into a Scheme Implementation Agreement with Lunit, Inc.
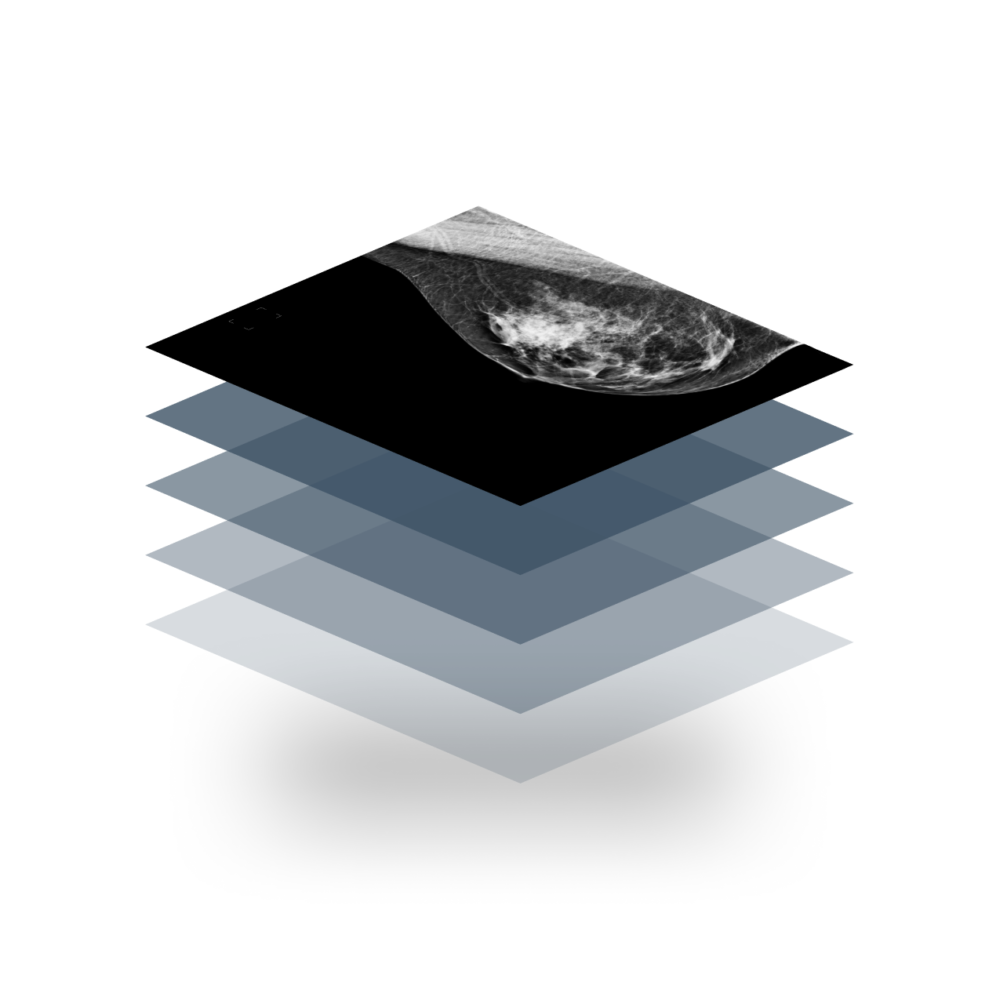
Clinically validated, AI-powered software for personalized screening and early detection of breast cancer.

2,000+

5,600+
“Volpara gives us confidence that we did the best possible job for our patients.”
– Deborah Hamel, Quality Assurance Manager, Derry Imaging

16.5 m+
“Knowing precisely how dense my breasts are gave me a clear path for screening.”
– Patient, Reno Diagnostic Centers
100 m+
“Every image we evaluate helps us evolve and improve our software, creating a path toward a healthier future.”
– Lester Litchfield, Head of Data Science, Volpara Health
Trusted by Healthcare Leaders







Get ready for 2024
January 1, 2024
New NAPBC Standards
The new NAPBC Standards Manual (2024) is a shift to more personalized care delivery with greater use of risk assessment and preventative protocols.
September 10, 2024
New FDA Density Rule
The Food & Drug Administration has updated the Mammography Quality Standards Act (MQSA) to make patient breast density notification a federal requirement.
What's New
Explore events, resources and viewpoints.
Blog

27 Jun 2023
Volpara is Microsoft’s 2023 Healthcare & Life Sciences Partner of the Year

FDA national breast density notification requirement



